Check out Mast Cell Activation Syndrome Resource Page for information on Mast Cell Activation Syndrome (MCAS), and what mast cells are. Mast cells are immune cells found in organs such as the liver, bone marrow, spleen, and skin. They are also found in the gastrointestinal tract and in the bone marrow. The main function of these cells is to protect the body from foreign invaders and to initiate the body’s inflammatory response to infection.
Do you have an autoimmune condition? If you do, the chances are you know just how frustrating it can be to live with your condition. MCS is a condition that can have a dramatic effect on the everyday lives of people with any type of auto-immune disorder.
Mast cell activation syndrome (MCAS) is a condition that can affect anyone, regardless of race, age, gender, or geography. Though it is more often seen in patients of Asian descent, people from all walks of life can suffer from this condition. MCAS is characterized by symptoms that include:
The following is a long summary that I put together by and for my own research. It is not meant to be medical advice, but rather an aggregation of resources and the self-experimentation I engaged during the long wait for a specialist appointment in this area.
I originally created the website since many other patients with CSF leaks (like I did) had asked me how they might reduce their responses after leak diagnosis or treatment. While having a CSF leak does not always mean you have a mast cell disease, the patients I’ve met are all complex cases like myself.
In those more complex instances, many people have a connective tissue problem that makes it more difficult to plug the leak. Many of these individuals have heightened food and environmental sensitivity, allergy, and systemic problems throughout the identification and treatment of their leaks, according to anecdotal evidence.
For me, the first inkling of these problems came when I was a kid. When I tried to sleep, I had a cough that itched my throat, and I couldn’t sleep through the night for a long time. When I reached adolescence, my irritating cough went away, but it reappeared when I became ill on the trans-Mongolian trains on route to Ulaanbaatar.
Following dengue illness in Vietnam, there were additional glimmers: itchy skin when I exercised, itching when I ate specific foods like blue cheese or drank red wine, and a first excursion into seasonal allergies in Oaxaca, Mexico during the first spring. My eyelashes were falling off because they were so terrible.
Of course, I had no clue what was going on, but following the spinal tap that caused my CSF leak, I came to the conclusion that mast cells were to blame. I saw a lot other leak patients with similar problems, did some research on dengue and mast cells (who knew!) and then it all came to a head when I had anaphylaxis during my fourth blood and fibrin glue patch and needed an adrenaline injection on the table.
Since the fibrin glue patch in early 2018, I’ve been focusing on controlling my “mad” mast cells.
What began as a reference website for other CSF leakers has evolved into a more in-depth examination of the various ways mast cells may impact the body. When the epidemic struck, scientists started looking at how mast cell dysfunction might be causing cytokine storms and protracted covid / PAS-C.
Prior to starting the regimen below, I had 24/7 searing and burning pain in my skin, nighttime adrenaline dumps that kept me up until 5 a.m. with heart racing, shaking with cold and low blood pressure, hives, heart racing, gastro-intestinal distress, and numerous instances of anaphylaxis in response to certain foods or smells. All of these symptoms have vanished since I started following the regimen I’ve outlined here, with the exception of occasional responses to new meals or odors. The disappearance of skin burning, as well as my ability to sleep again, was a huge relief.
Please use the contact link on the menu bar above to send me an email if you have any edits or more research to contribute to this page. I’ve visited a mast cell expert and had lab testing after creating this article in 2019, and I’ve been diagnosed with mast cell activation syndrome (MCAS).
Written in August of 2019; revised in June of 2024
BEGINNING AT THE TOP: WHAT ARE MAST CELLS?
Mast cells are immune system “sentinels,” a kind of white blood cell that aids in the regulation of immunological processes in the body. Because they live in tissues rather than the circulation, they are referred to as resident immune cells. They may be found in a variety of tissues throughout the body, including connective tissue, endothelial cells, epithelial cells, and even the brain.
Mast cells are immune system cells that reside in the bone marrow as well as internal and exterior body tissues such as the gastrointestinal tract, airway lining, and skin. Mast cells are found in everyone’s body, and they perform a variety of complicated and important functions in our overall health. They perform beneficial functions in our bodies by protecting us from infection and engaging in the inflammatory process. Mast cells, on the other hand, are involved in allergic responses ranging from a little swelling after a mosquito bite to life-threatening anaphylaxis.
The Mastocytosis Society of the United States (TMS) is the source for this information.
They’re crucial; we need them! – However, like with many other situations, when they get out of balance, things start to go wrong.
Mast cells that are overactive may cause a variety of issues and symptoms. Because mast cells are found throughout the body, the symptoms are often systemic. Because everyone of us has a unique immune system, the symptoms and manifestations of mast cell illness vary from person to person.
Mast cell degranulation is a term used to describe the process by which mast cells release their gran
As you can see in the image from the movie below, mast cells are packed with microscopic granules. When they get “mad,” they release up to 200 distinct signaling molecules – known as mediators – into the circulation, a destabilizing process known as degranulation. Those mediators are inflammatory, and the degranulation process sets off a chain reaction of inflammation that has the potential to disrupt other bodily functions. Mast cells are found in all organs and tissues of the body and play a role in allergy, immunological, and inflammatory responses.
We don’t want the mast cell’s capacity to degranulate to be lost. The degranulation reaction is part of the body’s natural defense when it detects intruders, and it helps keep us safe and healthy, as the quotation above shows.
The issue is that in mast cell activation syndromes, the body’s natural defense reaction goes haywire. Mast cells get enraged* and build a defense against things that aren’t a danger in the first place. Things that would not normally trigger an ATTACK! reaction in a ‘normal’ immune system now trigger an ATTACK! response in the immune system.
When exposed to a number of stimuli, such as excipients in medications, stress, and others, the normal mast cell function is disrupted, and the mast cells become hypersensitive and degranulate. Below, I go through the many kinds of triggers.
*Yes, mast cells are anthropomorphized. I find it useful to think of them as friends with whom I’m attempting to reach an agreement.
A brief video demonstrating what occurs when mast cells degranulate may be seen below:
Degranulation of mast cells may cause sensations of anxiousness.

Mast cell degranulation may also induce anxiety by releasing large amounts of meditators such as histamine into the circulation. When patients come with anxiety, sadness, or brain fog, according to a Psychology Today article, they should be checked for mast cell dysfunction.
Patients who present to their primary care doctor with a slew of seemingly unrelated dramatic complaints affecting unrelated organ symptoms, many of which include prominent psychiatric symptoms, are frequently misdiagnosed as suffering from a psychosomatic condition and told, “It’s all in your head.”
They may be sent home with an antidepressant or anti-anxiety prescription, which not only feels invalidating, but also fails to treat the underlying source of their problems. Detecting MCAS as the cause of symptoms has significant therapeutic implications and may help you recover faster.
In addition, according to a 2017 case report titled “Mast cell activation disease masquerading as a neurological breakdown,” a patient who came with significant mental symptoms was really diagnosed with MCAS, and his neuro-psych symptoms disappeared after the mast cells were stabilized. “Some individuals may show with mild neurocognitive abnormalities as well as frank psychotic behaviors,” according to the same study.
Those mast cell patients I’ve talked with have told me that after their mast cells were stabilized, their anxiety levels dropped dramatically, including several who experienced a “sense of dread” that accompanied severe worry. Controlling mast cells calmed my racing thoughts before bedtime; it turned out that the source of my worry wasn’t stress after all.
BEYOND HISTAMINE INTOLERANCE: THE BASICS OF MAST CELL DYSFUNCTION
The growth and accumulation of sensitized/altered mast cells, as well as the improper release of mast cell mediators, are the root causes of all mast cell disorders, resulting in symptoms in various organ systems. Mast cell activation syndrome, mastocytosis, and the newer Hereditary Alpha Tryptasemia Syndrome are the three major types of mast cell disorders (HATs).
Mast cell diseases can cause tremendous suffering and disability due to symptomatology from daily mast cell mediator release, and/or symptoms arising from infiltration and accumulation of mast cells in major organ systems. Although systemic mastocytosis is a rare disease, those suffering with MCAS have recently been increasingly recognized and diagnosed.
As a result, patients with MCAS appear to represent a growing proportion of the mast cell disease patient population. It is important to note that the process of mast cell activation can occur in anyone, even without a mast cell disease, as well as in patients with both mastocytosis and MCAS. – The Mastocytosis Society of the United States
This article focuses on mast cell activation disorder (MCAS), which occurs when mast cells become hyperactive and degranulate excessively. According to a research published in April 2024, “this illness may impact up to 17% of the population, with symptoms ranging from moderate to severe.” Because of a lack of provider knowledge, MCAS is often misdiagnosed or identified late.” MCAS is often a lifelong issue, like my childhood glimmers, that is accelerated by trauma, viruses, and other factors.
Mastocytosis, as previously mentioned, occurs when a patient has an excessive number of mast cells and is prone to degranulation. Mastocytosis, which comes in a variety of forms, is often verified by a bone marrow biopsy that searches for a mutation in the KIT gene. Mastocytosis is often characterized by a rapid onset or precipitating event.
Mastocytosis comes in a variety of forms, the most prevalent of which are cutaneous mastocytosis and systemic mastocytosis. Mastocytosis is diagnosed in the following way:
- The presence of typical skin lesions and a positive skin biopsy showing characteristic clusters of mast cells are used to diagnose cutaneous mastocytosis.
- A bone marrow biopsy is typically used to detect systemic mastocytosis. The WHO has set diagnostic criteria, which include a main criterion of a particular density of mast cells, as well as minor criterion such as a KIT D816V mutation, serum total tryptase, and other factors.
Then there’s Histamine Intolerance, which, according to my mast cell expert, is just a lesser form of MCAS. Others think it stems from microbiota or gastrointestinal problems, as well as genetic concerns that cause a shortage of DAO in the body, an enzyme that aids in the breakdown of histamine.
Histamine intolerance is linked to both the DAO and HMT pathways, and some medicines and foods may decrease DAO levels. Taking supplementary DAO and following a low histamine diet, according to Dr. Joneja, may assist these individuals (see my suggestions in the “treatment organically” section below). If you think your problem is histamine intolerance rather than MCAS, check out Dr. Joneja’s PDF introduction here.
Mast cell disorders, on the other hand, are more than just histamine; the mast cells produce 200 different mediators, histamine being only one of them. In cases when DAO and reduced histamine diets are inadequate, in-depth mast cell testing may be considered.
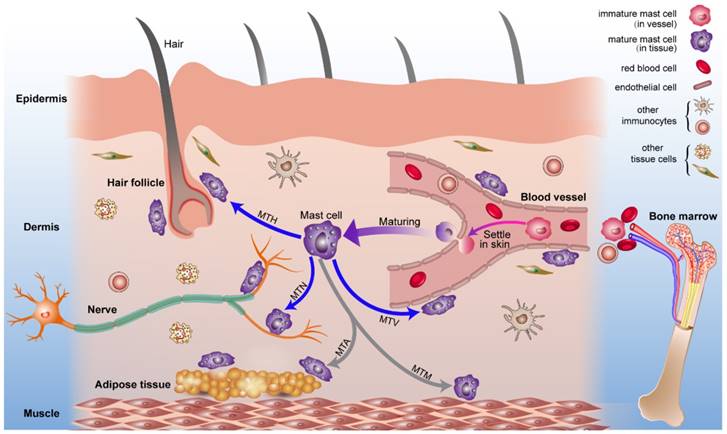
This image below from a January 2024 study “Mast Cells: Fascinating but Still Elusive after 140 Years from Their Discovery,” is also a helpful pictorial demonstration of the many conditions that can arise when the normal mast cell process gets dysfunctional.
Mast cells have been linked to a broad range of diseases, as seen in this diagram.
Here are the complete citations from the study:
The broad range of pathophysiological situations in which mast cells and their mediators have been involved is shown in this diagram. Mast cells have long been thought to have a proinflammatory role in allergic diseases including bronchial asthma, allergic rhinitis, urticaria, food allergy, anaphylaxis, atopic dermatitis, and angioedema.
Mast cells have emerged as a key cell during bacterial, fungal, viral, and helminth infections during the past several years. Mast cell-derived mediators have been shown to defend against a variety of venoms in elegant investigations. Mast cells and their mediators are thought to have a role in a variety of features of tumor start and development, probably through producing a variety of angiogenic and lymphangiogenic components.
Systemic mastocytosis is a clonal illness caused by a somatic gain-of-function mutation in the KIT gene. Mast cells are engaged in various stages of atherosclerosis and myocardial infarction and are strategically positioned in distinct regions of the human heart and atherosclerotic plaque. Rheumatoid arthritis, celiac disease, multiple sclerosis, and bullous dermatoses are among autoimmune diseases in which these cells play a role.
Stress, pain, pruritus, and inflammatory bowel disorders are all linked to mast cell–nerve communication.
MCAS Overview Posts for Further Reading:
- Clinical Manifestations of Mast Cell Activation Syndrome By Organ Systems, by Dr. Lawrence Afrin and Dr. Tania Dempsey, is a comprehensive symptom list.
- When Histamine Goes Haywire, by Jill Carnahan, is a great review of mast cell activation.
- MCAS, When The Immune System Runs Amok, is available at the Hoffman Center. You may find their MCAS questionnaire here.
- Mastocytosis, cutaneous masto issues, and mast cell activation syndrome are all defined in this PDF from the Mastocytosis Society. (This is a link to a PDF that you may download to your computer from my Dropbox.)
- Dr. Maitland’s presentation “Living With Mast Cell Activation Syndrome” was given at the Ehlers Danlos Global Learning Conference in 2018.
Nerves and Mast Cells
Many research have been done on the relationship between mast cells and nerves in most tissues, including studies that indicate mast cells are continuously sending information to the neurological system. Mast cells may also be found in connective tissue and mucosal surfaces, where they interact with their surroundings in a variety of ways. They have a variety of roles as well; they’re believed to play a key part in infection resistance and are engaged in inflammation and tissue healing after an injury. They’re also found in hair follicles!
This is just the top of the iceberg. Patients travel to various experts with apparently no similarities in their symptom profile, only to find out later that the mast cells, which are found all throughout the body, are the cause.
Mast cells may produce a wide range of pro- and anti-inflammatory mediators, including cytokines, growth factors, and arachidonic acid metabolic products. Histamine, serine proteases, proteoglycans, sulphatases, and tumour necrosis factor (TNF) are among the mediators that are produced minutes after the cell degranulates.”
In the Significance of Conversation between Mast Cells and Nerves, there is a comprehensive study/explanation of mediators.
MCAS EXPLAINED TO FAMILY AND FRIENDS
How you express your demands and/or explain the illness to family and friends is one of the difficulties of having a systemic, complicated sickness.
Traditional allergies, which are detailed below and consist of an allergen that is a continuous trigger, frequently increasing with each exposure, are known to most individuals. Given the systemic nature of mast cell illness, it’s less black-and-white and less “I’m going to die if I come into touch with this item” — but mast cell patients with IgE allergies do exist. For example, I carry an EpiPen since I am allergic to bee venom. This is a constant allergy with a high risk of anaphylaxis, so I have to be cautious.
Mast Cell Activation Syndrome’s Bucket Analogy
I also have mast cell activation syndrome, which causes responses all throughout my body–sometimes even anaphylaxis–but is caused by a number of variables that all funnel into my immune system. A bucket analogy is often used.
Here’s how I use it to explain what’s happening:
Consider a bucket that receives water from a variety of sources. The majority of individuals have a drain that works and is completely open. I have two issues: my drain is very blocked, and a lot of water is pouring into the bucket. Even a drop of additional water will cause the bucket to overflow while it is already overflowing.
Gastro problems, itching, nausea, bone pain, and a variety of other symptoms may occur as a result of overflow.
As a result, my objective is to maintain my water levels as low as feasible. To do so, I eat a low-histamine diet (which helps reduce water flow into my bucket), take mast cell stabilizers and antihistamines (both of which assist), and take DAO (a histamine-breaking enzyme) with meals, which helps clear the drain a little bit.
However, regular calibration and calculus are required to ensure that the water level remains low and the drain remains clean.
Unlike IgE allergies, living with MCAS feels like you’re always using an abacus. Is this something you can eat? So, how stressed are you at the moment? Is there a lot of pollen in the air? What’s the total number of mast cell stabilizers you’re taking? It’s a lot of spinning plates to keep track of, but it becomes a lot simpler if you stop trying to create binary rules and instead allow yourself to investigate the triggers you may have with interest rather than hatred. Some things will always make you respond, while others will only make you react based on how full your “bucket” is.
I strongly advise you to acquire a notebook and keep account of everything you eat, supplements or medications you’re taking, changes in your surroundings, and your symptoms in order to narrow down what your particular triggers are.
To assist simplify the concept and list out what has worked for myself and many other patients, I created this “bucket” infographic:
Yes, I had a good time creating this infographic.
MAST CELL ACTIVATION SYNDROME SYMPTOMS AND TRIGGERS
Mast Cell Activation Disorder: What Are the Signs and Symptoms?

Because mast cells are found in so many tissues and systems throughout the body, when they degranulate, a wide variety of symptoms may ensue.
- The face, neck, and chest are all flushed. Itching and/or rash
- Hives, rashes, and more may be found in TMS’ “visual guide to skin lesions” here.
- Eczema and atopic dermatitis (see here, and here.)
- Angioedema is a condition in which the skin becomes swolle (swelling)
- Itching and congestion in the nose
- Shortness of breath and wheezing
- Itching and swelling in the throat
- Headaches
- Anxiety or sadness may accompany brain fog and cognitive impairment.
- Diarrhea, nausea, vomiting, stomach discomfort, bloating, and gastroesophageal reflux illness are all symptoms of gastroesophageal reflux disease (GERD)
- Osteoporosis, osteosclerosis, osteopenia, and osteoporosis are all conditions that affect the bones and muscles.
- Syncope/fainting, light-headedness
- Chest discomfort, rapid heart rate
- At the onset of a response, blood pressure may be low or high.
- blood pressure instability as a result of a response
- Cramps or bleeding in the uterus
- Tinnitus (ringing in the ears)
- Dermatographism (writing on your skin with a fingernail or a blunt instrument, creating a red welt – more information here.)
- Edema is a condition in which the body’s (fluid accumulation in different parts of body)
- Wound healing is slowed
- Interstitial cystitis is a kind of cystitis that affects the bladder
- Dentin and tooth deterioration
- Wonky liver enzymes are common (High bilirubin, elevated liver enzymes, and high cholesterol)
- Fog in the head
- Coagulation problems and blood disorders (clots, DVT, easy bruising, heavy periods, nosebleeds, and/or wounds that won’t close up)
This chart may be downloaded by clicking here.
The particular mast cell mediator that is released into your circulation, as well as its potential consequences:
Flushing, itching, diarrhea, hypotension, panic attacks/anxiety are all symptoms of histamine. Shortness of breath due to leukotrienes Flushing, bone pain, mental fog, cramping are all symptoms of prostaglandins. Osteoporosis and skin lesions are caused by tryptase. Fatigue, weight loss, and swollen lymph nodes are all symptoms of interleukins. Heparin: Osteoporosis, clotting/bleeding issues Fatigue, headaches, and bodily pains are all symptoms of tumor necrosis factor.
What Are Some Mast Cell Activation Syndrome Triggers?
Food, activity, environmental exposure, and trauma are all potential triggers for mast cell degranulation. It’s hard to fathom how such diverse and apparently harmless factors (vibration?!) may degranulate mast cells, yet that’s exactly what happened.
The Mastocytosis Society, the Canadian Mastocytosis Society, and blogs have all contributed to the following list:
- a strenuous workout
- Heat, cold, or temperature swings are all examples of temperature variations.
- Sun/sunlight
- Fatigue
- Stress
- Affective (trauma, loss, abandonment)
- Physical (pain, accidents, and medical treatments, for example). See this 2019 PDF document to bring to the hospital that covers mast cell diseases, phases of anaphylaxis, and triggers for medical treatments.)
- Environmentally friendly (weather changes, pollution, pollen, pet dander, mold, gas leaks)
- Foods or drinks with a high histamine content. For additional information, see the diet lists under TREATING MCAS. Many of the items on the histamine “no” list are actually highly suggested for autoimmune diets – for example, fermented foods/natural probiotics, spinach, etc. – which can exacerbate MCAS symptoms for many individuals.
- Yeast
- Alcohol
- Dairy products (especially fermented dairy like kefir, blue cheeses, or aged dairy like Parmesan cheese)
- Gluten
- Fermented foods (particularly sauerkraut, kombucha, miso, kimchi, fish sauce, and soy sauce – essentially anything that imparts a delicious umami flavor to food)
- Meats and fish that have been cured and smoked
- Shellfish
- Fruits of the citrus family
- Vinegars
- Fruits and vegetables that are overripe
- Leftovers (I can have supper stuff for lunch the following day, but that’s all.) I usually simply freeze it and consume it straight away, which prevents the aging/histamine breakdown process.
- Strawberries, in particular,
- Spinach
- Various than pure dark chocolate, there are other types of chocolate.
- Tomatoes
- Certain food additives (see here for more)
- There are a remarkable number of medicines. Some of the items listed below are on the ‘avoid’ list. A larger list may be found here and here. Meditation is also on the later list, which may help to relax mast cells.
- Amphetamines
- Aspirin
- Dextromethorphan is a kind of dextromethorphan (cough suppressant)
- Dipyridamole is a kind of dipyridamole that is (Persantine)
- Antifungal medications
- Lidocaine, for example, is a local anesthetic (any amino amide-type)
- Dexamethonium, Gallamine triethiodide, and other neuromuscular blocking drugs (all)
- NSAIDs (nonsteroidal anti-inflammatory drugs) (Non-steroidal anti-inflammatories: Advil,Motrin,etc)
- The majority of opiates (codeine, morphine, Percocet/Oxycodone, and so on) are addictive.
- Hydrochloride of thiamine (A form of vitamin B1)
- Hydrochloride of tolazoline
- Trimethaphan, Trimethaphan, Trimethaphan, Trimethaphan, Trimethaphan
- Contrast dyes are utilized in MRIs, CT scans, and other imaging procedures.
- Friction or mechanical irritation (rubbing/chafing)
- Vibration
- fragrances from nature (strong natural scents like essential oils, environmental smells)
- noxious odors (cleaning products, for example, or perfumes)
- Infections (viral, bacterial, or fungal infections may exacerbate MCAS and should be treated with caution with the assistance of your doctor – see below for more information, including the picture I provided)
- Venom is a poison (bees, wasps, spiders, snakes, etc.)
- Diesel is a kind of fuel (smell)
Mast Cell Problems Can Be Caused by Viruses
Mast cells are engaged in the body’s regular virus-clearing activities, but chronic infection or contact with other elements of the immune system, such as with COVID-19, may create long-term mast cell issues (see below).
For example, having dengue illness from a mosquito while traveling sparked everything for me as an adult. A number of research have been conducted on the function of mast cells in dengue infections, including one that states:
Mast cells, which are immune cells, may obstruct rather than assist the body’s response to the dengue virus, suggesting that mast cell products might be utilized as biomarkers to detect severe cases of the illness.
“The response of mast cells to dengue virus can be beneficial or detrimental. When a mosquito injects dengue virus (brown hexagons) into the skin, the viruses are detected by specific antibodies (green) or unidentified receptors (blue) on the surface of resting (i.e., non-activated) mast cells.
These can then trigger an anti-viral response (left) by releasing the contents of their granules (degranulation) and by upregulating intracellular anti-viral molecules (RIG-I and MDA5). The activated mast cells also secrete signaling molecules called chemokines, which recruit other immune cells including natural killer cells (NK), natural killer T cells (NKT) and T cells, which help to clear the virus.
However, if local control mechanisms fail, the virus will enter the bloodstream and be carried to other organs (right). This activates the mast cells in these organs so that they undergo degranulation, releasing ready-made proteases such as chymase and tryptase, and synthesizing inflammatory mediators (leukotrienes and vascular endothelial cell growth factor [VEGF]).
These increase the permeability of capillaries, leading to vascular leakage. Mast cells in these organs can also be activated by endogenous inflammatory mediators (such as C3a and C5a) that help the body to remove pathogens. Blocking mast cells (or their mediators) with drugs such as cromolyn, ketotifen and montelukast reduces pathogenic vascular leakage, but might also hamper viral clearance. Anti-mast cell therapy could thus be a double-edged sword.”
Mast cells may be a double-edged sword in viruses, as the caption on the (ADORABLE) picture points out, since we want them to perform their job and clean out a virus, but when they are defective, they overdo it. (And, according to the research, suppressing the immune response in non-MCAS patients may hinder them from completing their job of removing the virus entirely.)
Mast cell activation may also be helpful in the case of influenza, according to studies. According to a research in mice titled “Mast Cell-Induced Lung Injury in Mice Infected with H5N1 Influenza Virus,”
A combination of ketotifen and oseltamivir, a neuraminidase inhibitor, protected all of the mice against mortality after infection. To summarize, our findings indicate that mast cells play an important role in the early phases of H5N1 influenza virus infection and provide a novel strategy for combating highly pathogenic influenza virus infection.
All of this is to imply that if you have a virus like COVID-19, dengue fever, influenza, or other infections, your mast cells may be activated. It may be more difficult to heal if you are genetically predisposed to mast cell issues. As a result, treating mast cell activation may possibly reduce the severity of infections, but we don’t want to go too far (at least in dengue).
MAST CELL ACTIVATION SYNDROME DIAGNOSIS
As I previously said, mast cell activation syndrome (or a sister disease such as mastocytosis or HATs) is often misdiagnosed owing to a lack of understanding of the condition’s origin and/or certain practitioners evaluating just a small number of meditators or only detecting igE allergies.
Furthermore, the lab tests needed to identify MCAS must be handled with extreme care and kept cool. Urine testing specimens must also be kept cool at all times. As a consequence, multiple rounds of testing may be required to validate the lab findings, which may be very inconvenient.
The practitioner will typically do a differential diagnostic analysis to rule out other inflammatory immunological diseases or mast cell disorder mimics. Symptoms are also so bio-individual that it’s far more difficult to pinpoint a diagnosis than, example, a disease that can be diagnosed with a simple gene test. The laboratories listed below do tests to determine the ranges of certain mast cell mediators, however experts point out that there are hundreds of mediators produced by mast cells in total, but only a handful have lab tests to quantify them.
Many mediation tests are not performed (or cannot be ordered) by physicians in Canada because they are costly and not funded by government healthcare. Some private mast cell practitioners, as well as mast cell experts in the United States, will cover them.
What Labs Do Mast Cell Activation Syndrome Tests Require?
Standard testing for MCAS includes both urine and serum (blood) tests. It can sometimes involve biopsies of the GI tract or colon. As stated earlier, samples can degrade really quickly at room temperature, and must be handled properly or else they will become corrupt. The mast cell doctor I saw said that laboratory or patient handling mistakes accounts for a lot of the false negative testing he sees, and he only works with specific labs that he knows he can trust to properly chill the samples.
The tests that the doctor ordered for me to see whether I had mast cell activation syndrome were as follows:
MCAS blood tests are available.
- A complete blood count (CBC) with a platelet differential is performed.
- Blood, histamine
- Plasma, histamine (chilled)
- Plasma, PGD2 (chilled)
- Metabolic Panel (Comprehensive)
- Assay for plasma prostaglandin D2
- PT + PTT
- Assay for heparin
- Anti-Xa heparin level in plasma (anti-Xa for unfractionated heparin, chilled)
- Serum, Tryptase
- Serum, Magnesium
- Urticaria Index for Chronic Urticaria
- Antibodies against IgE
- Chromogranin-A
MCAS testing in the urine
- 24hr Urine, Chilled Histamine
- Random Urine, Histamine (then chilled)
- Prostaglandin D2 is a kind of prostaglandin that is found in the urine at random (then chilled)
- Urinary prostaglandin D2 that has been chilled for 24 hours
- 2,3-dinor-11-beta-prostaglandin-F2-alpha is a random urine 2,3-dinor-11-beta-prostaglandin-F2-alpha (then chilled)
- 2,3-dinor-11-beta-prostaglandin-F2-alpha urinary 2,3-dinor-11-beta-prostaglandin-F2-alpha
- N-methylhistamine in the urine at random (then chilled)
- N-methylhistamine in urine, chilled for 24 hours
- Leukotriene E4 is a kind of leukotriene that is found in the urine at random (then chilled)
- Leukotriene E4 urinary leukotriene E4 urinary leukotriene E4 urinary leukotriene E4 urinar
DNA Tests
Important information regarding mast cell testing: read before you test!
- For testing purposes, you should not be asked to stop taking your antihistamines. Some physicians in Canada insist on it. The majority of mast cell experts in the United States do not. Antihistamines will not alter the findings of serum and urine tests, according to mast cell specialists, since they simply block the body’s receptors.
- For testing, some physicians may ask you to stop using mast cell stabilizers. One week before to testing, I stopped taking quercetin, PEA, Vitamin E, and the other stabilizers mentioned above, as well as anything that impacted inflammation.
- If you use NSAIDs like Advil, you should stop taking them 5 days before your test.
- If you use PPIs (proton pump inhibitors), you should stop taking them 5 days before your test.
- A remark on tryptase: even during flares, most mast cell patients with MCAS (not mastocytosis) test normal for tryptase. This is why healthcare providers should look for various mediators. However! If your tryptase level is high, you might consider a gene test for HATs, or hereditary alpha tryptasemia syndrome, a relatively novel mast cell disease. Because it requires a saliva gene panel, which can be obtained online through Gene By Gene, it is a simpler condition to rule in or out.
- Mastocytosis (but not all instances) and HATs both have increased tryptase levels. Because MCAS is a relatively new illness, some allergists or immunologists may test tryptase and conclude that it is not MCAS if the results are negative. That does not seem to be the case among mast cell specialists, even among those who include tryptase in the diagnostic criteria. MCAS cannot be ruled out only on the basis of tryptase tests.
- There are presently two “consensuses” of diagnosis among mast cell specialists, both of which are recognized by the World Health Organization. Drs. Afrin, Molderings, and others are part of one group. Drs. Valent, Akin, and others make up the second group, which may be found here. The second group is more interested in tryptase, while Dr. Afrin’s is not**. Both sides are certain that they are right.
- A word on the differences between IgG and IgE reactions: IgG and IgE tests for food allergies and allergies are often misunderstood. They have anything to do with mast cell activity, but they aren’t a reliable test for mast cell activation. IgE allergens may cause mast cell degranulation, so yes. However, IgE testing (which is often performed by an allergist) is not utilized to diagnose MCAS. You can have MCAS even if you don’t have any IgE allergies. Many mast cell sufferers, on the other hand, struggle with dermatographism, or the inability to write on their skin. I can write my name on my skin with ease, and it will glow puffy and red for a long time. Skin IgE testing may only reveal responses to the scratches, not the allergen; it is ineffective for MCAS.
- Mast cells contain IgE and IgG receptors, and both kinds of antibodies may cause greater histamine levels or higher levels of other meditators, as well as induce degranulation.
- IgG responses are the more tranquil of the two, but they may still cause anaphylaxis-like symptoms. These antibodies are prevalent not just for infections that harm us, but also for food-related problems when we have GI permeability disorders (leaky gut and more).
- IgE responses, on the other hand, are typically acute and quick, similar to when we are stung by an allergen. It’s a rapid degranulation reaction by the immune system’s sentinels in an attempt to guard against anything important. Despite the fact that they are not part of MCAS testing, they may be helpful. If you’re testing IgG, it’s critical to utilize IgG antigen testing, then phase out those meals for a few months to see if it makes a difference, then attempt to reintroduce with nutritionist assistance.
**Drs. Afrin and Dempsey replied to remarks regarding why tryptase should not be a trustworthy / gold standard marker for diagnosing mast cell activation syndrome as follows, although experts continue to disagree:
- We (Dr. Dempsey and Dr. Afrin) have not observed an increase in tryptase to be a reliable sign of mast cell activation in our combined clinical experience of many thousands of MCAS patients. A persistently elevated tryptase level may be a reliable marker of an increased number of mast cells in a person, and a clear, brief spike in tryptase over some lower, stable baseline level probably represents a brief flare of mast cell activation, but such a spike is not a reliable marker of mast cell activation. Indeed, it appears that mast cells can be activated in a variety of ways, releasing a variety of mediators under a variety of conditions, making it difficult to imagine how a spike (of any magnitude) in just one mast cell mediator could be a truly reliable marker of mast cell activation detectable in the majority of activation events in most people. During instances of blatant mast cell activation, such as anaphylaxis, we’ve observed numerous individuals whose tryptase levels have gone *down*. And we’ve observed that in individuals with symptoms that point to mast cell activation, increased levels of mast-cell-specific mediators other than tryptase are nearly invariably detected in the blood and/or urine.
A SUMMARY OF HOW I MANAGED TO CONTROL MY MAST CELLS

The level of pain I was with the CSF leak and the (unknown to me at the time) mast cell dysfunction was debilitating. It got to a point where I simply sobbed in bed all day long. When my research led me to suspect a mast cell disorder, I implemented the following steps. They sharply reduced my pain levels while I waited for specialist testing.
** This is just what has worked for me in the past and is not intended to be medical advise.
FIRST, I identified triggers in my surroundings and eliminated them, such as highly scented household cleaners, non-natural cosmetic goods or shampoos or face washes (see below for brands I use), and others. Second, for two weeks, I followed a rigorous low histamine diet, avoiding alcohol, cold cuts and smoked/cured meats, canned fish, anything pickled or fermented, aged cheese, overripe vegetables, gluten (which I already avoided since I’m celiac), citrus fruit, yeast, soy, and tomatoes. I also stopped eating leftovers that were more than a day old and began freezing everything I prepared for later use. The whole list of things to eliminate may be seen in the diet list below. Then I gradually introduced some of the medium histamine items. THIRD, natural mast cell stabilizers such as quercetin and PEA were introduced. What I utilized is detailed in the procedure below. FOURTH, make additional lifestyle adjustments such as a) limiting inflammatory foods and beginning DAO, the enzyme mentioned below, 15 minutes before eating higher-histamine meals, and b) lowering stress via meditation. Corticotropin hormone (CRH), a powerful mast cell degranulator, may be reduced by reducing stress. FIFTH, I began testing with H1 antihistamines to see if they might assist. I stopped using an H1 after two weeks if it didn’t work or make a significant impact. MCAS patients are typically given H1s every 12 hours to establish a “histamine blockade,” which is more often than non-MCAS patients are given H1s. SIXTH, when I found “my” H1 antihistamine, I began experimenting with H2 antihistamines. These, like H1s, should be dosed every 12 hours. I haven’t found one that works for me yet, but I’m working on it. SEVENTH, I performed a stool test and specialized blood testing to make sure any of my mast cell problems weren’t caused by parasites or viruses. I understand that this testing is not available to everyone.
When introducing new vitamins or medications, it was critical to start slowly and gradually. Know that determining the item or chemical you respond to may be difficult at times. Because specialists have made it apparent that excipients/fillers in medicine, not the drug itself, are frequently what mast cell sufferers respond to, I now have a lengthy chart where I put in the things that works for me and its fillers. (Recognition and Management of Medication Excipient Reactivity in Patients With Mast Cell Activation Syndrome, a 2019 review paper, has more on excipients in fillers.)
It wasn’t pleasant or simple, but it kept me afloat until I could see a mast cell expert since I didn’t have access to competent medical care.
NATURAL MAST CELL ACTIVATION TREATMENT
Eliminating Triggers to Reduce Histamine
The term “reduction of triggers” refers to any triggers you have from the lengthy list I provided before. This entails eliminating not just environmental irritants such as shampoos and soaps, but also consuming a low-histamine diet in order to reduce circulating histamine levels in the body. While some physicians do not advocate a low histamine diet, I know that I cannot control my responses and symptoms without severely restricting my food consumption.
(My blood tests also revealed an extremely high amount of circulating histamine–one of the highest my practitioner had ever seen; I’m an overachiever, eh?)
Because vibration is a trigger for many people, vehicle trips, electric toothbrushes, and other things may cause mast cells to degranulate. Many essential oils have an overpowering smell that causes discomfort.
Diets that are low in histamine and other diets that may help with MCAS
There are just a few mast cell sufferers. I’ve talked with people who eat a healthy diet. This aspect is difficult for me as a former food/travel writer. I joke that I’m the worst food writer ever, but the reality is that after dealing with celiac disease for 20 years, I’m no stranger to taking things out rigorously and methodically. I had no idea I’d have to make so many sacrifices!
Because it lowers the quantity of histamine floating about, a low histamine diet may help lessen the overall load on your body. It may also assist non-MCAS patients with itching or asthma.
Low histamine is combined with low oxalate (which is particularly important for individuals with pelvic inflammation or interstitial cystitis) and low FODMAP.
Here are a few diet programs I found on the internet:
- Swiss SIGHI lists have low histamine levels. Here are some suggestions for an elimination diet. A lengthy PDF of graded histamine levels in foods/additives, etc. may be found here.
- Alison Vickery has a low histamine level. Here’s a link to her DIET PDF. She employs a functional approach that incorporates both naturopathic and allopathic treatment, and she properly references her sources. This low histamine diet list has the most closely matched how my body responds to certain meals of all the low histamine diet lists.
- Beyond low histamine: Some individuals with Ehlers Danlos syndrome or auto-immune diseases like Crohn’s disease or colitis have difficulty digesting meals that aren’t low in histamine. See this page for more information on those extra limitations, as well as a low histamine diet recommendation list for individuals who must consider other factors.
- These include lectins, oxalates, salicylates, sulfur, and FODMAPs, all of which may impact MCAS depending on the individual. Higher-doses of Vitamin C will be a concern if oxalates are an issue. To be able to pinpoint triggers, it’s critical to maintain track of data linked to diet and supplements.
- Lectins are proteins present in certain plants that, according to early studies, may also activate mast cells. See here for a list of low-lectin foods.
- Vitamin C contains oxalates, which is a problem since high-dose vitamin C is beneficial for mast cell stability and collagen production. I had to reduce my oxalate consumption, which I had no idea was making my problems worse. There are numerous oxalate food lists online, but this one is a good place to start.
- When it comes to FODMAPS, a reduced FODMAP diet may help to lower histamine levels in the bloodstream.
- Here are a few useful smartphone apps: Baliza is a German business that has created numerous low histamine diet applications that are updated when new facts and research become available.
- Food Intolerances: The software is very comprehensive, allowing you to sort by various food intolerances or allergies. Histamine, fructose, sorbitol, gluten, lactose, and FODMAPs are all measured. Here’s the Apple Store, and here’s the Google Play Store.
- OxiPur: Measures oxalate and soluble oxalate in foods, is searchable and sortable by food category, and provides certain oxalate-related data, such as calcium in each meal. This is an Apple-only zone.
- Histamine Info is an app that utilizes the Sighi list and is updated on a regular basis. This is an Apple-only zone.
Mast Cell Activation Syndrome Supplements

(I’ve included studies to back up why I take each of these supplements.)
- DAO (Diethylamine Oxidase): DAO is an enzyme generated naturally in the body that aids in the breakdown of histamine from meals. Other individuals have genetic variations that reduce DAO synthesis, some people consume diets high in items that reduce DAO, and some people just need more DAO to help them cope with the consequences of high circulating histamine levels. There are two products on the market that are (in my view) reliable for DAO, and I use the Seeking Health version since the other one (Umbrellux) altered their composition and no longer works for me. This DAO is made from porcine sources and should be consumed within 10-15 minutes after a high-histamine diet.
- (non-gmo, pharmaceutical quality) Vitamin C Nutribiotic Ascorbic Acid Powder —
- Sodium Ascorbate Vitamin C Nutribiotic (non-gmo, pharmaceutical grade). I include sodium ascorbate in my supplements / total Vitamin C count because there is some evidence that it helps the extracellular matrix.
- Organic and freeze-dried Camu Camu. Vitamin C’s preferred mode of transport. If you have an oxalate problem, you should restrict your vitamin C consumption. This is bad since Vitamin C may assist decrease histamine levels and regulate the body in various ways, but mast cell problems are a tangle of catch-22s.
- Microingredients that aren’t genetically modified Sephora Japonica buds contain quercetin. Jarrow Formulas Quercetin, Cardiovascular Support, 500 mg is a good option if you like capsules. To aid absorption, Quercetin should be taken with fat. The Thorne Quercetin Phytosome is a more bioavailable form of quercetin. The quercetin absorbs better thanks to the phytosome formulation, which is in this instance linked with sunflower lecithin.
- Zeolite is a mineral that is used in functional medicine. Doctors think that zeolite may aid in the removal of histamine from the body by acting as a binder for the histamine. For certain metals, zeolite is also employed as a binder.
- NasalChrom: For seasonal allergies and food responses that include nose running/itching in the face, use NasalChrom. Mast cell stabilizer sodium cromlyn
- Zatidor eye drops include ketotifen fumarate, a powerful mast cell stabilizer; if you can’t get your hands on tablets or compounded ketotifen, eye drops may be a good alternative.
- PEA stands for palmitoylethanolamide, which is pure and comes from a trustworthy source. PeaCure and Vitalitus are two businesses in which I have faith. PeaCure has been unavailable for some time, however Vitalitus is now available and shipping to Canada. When selecting a brand, check sure the supplement has been micronized to tiny diameters; this is the form in which studies have shown it to be beneficial. PeaCure has the lowest diameter (they’re ultra-micronized), whereas Vitalitus is micronized to less than 5 micrometers and makes an excellent backup.
- The magnesium I use is Magnesium L– Threonate. The Doublewood brand has elicited no negative responses and is accessible in the United States and Canada.
- Thorne Soy Free Meriva is the finest Curcumin for mast cell sufferers that I’ve discovered. It is soy-free and contains sunflower lecithin to aid bioavailability. It’s also composed entirely with curcumin, so it’s free of the higher-oxalate turmeric. Black pepper extract is used in many other products in this category to aid absorption, but this is a mast cell degranulator. Meriva is an excellent choice for people who wish to give it a go.
- luteolin with rutin powder LutiMax (NOTE: This is NOT Lutein! It has to be luteolin. Neuroprotek, a Dr. Theoharides supplement from his Algonot business, is another choice for luteolin, rutin, and quercetin. Profits go toward future research.)
- If you wanted to mix the two, you might use Mirica® – Pea (Palmitoylethanolamide) and Luteolin – Natural Pain Relief – Made with OptiPEA® from the Netherlands (Luteolin and PEA). Although I do not do so, it is an alternative. The PEA has been micronized rather than ultra-micronized.
- Premium Black Seed Oil from Amazing Herbs is organic and cold pressed.
- PROBIOTICS:
- Essential Nutrients 400 IU Vitamin E (Mixed Tocopherols) (NOT soy free) OR, if you’re like me and don’t only want one tocopherol but also tocotrienols, try Healthy Origins Tocomin SupraBio (Tocotrienols) 50 mg. (This recipe is soy-free.) 1 in the morning and 1 in the afternoon)
** Please note that the Amazon links above, as well as the others on Legal Nomads (see the bottom for more), are affiliate links, which means I get a small fee on certain transactions.
PROTOCOL I’M USING RIGHT NOW
- 5mg H1 taken twice a day, at 10 a.m. and 10 p.m. (levocetirizine). Because medication is not available over the counter in Canada, I had to have it compounded. For me, it’s the greatest H1, but everyone is different. Furthermore, many individuals are allergic to excipients in medications, necessitating compounding. Compounding using Avicel, a hypoallergenic filler, or rice flour or baking soda is the most common method. To discover more about your choices, contact a compounding pharmacy near you.
- Pure powdered Quercetin (MicroIngredients) – 1 scoop 500mg, 1x per day
- Lunchtime 0.5mg ketotifen
- 2 pills of quercetin phytosome with supper
- 1x AM, 1x with lunch PEA (PeaCure or Vitalitus brand)
- 250 mg vitamin C, taken once a day (camu-camu is what I use most)
- 1 scoop (150mg of each in 1 scoop) luteolin/rutin powder before bed, as required
- 1x DAO for lunch and 1x DAO for supper
- 2 capsules Magnesium L-Threonate in the late afternoon
- 1 vitamin E capsule with lunch, 1 capsule with supper
- 1 vitamin D (1000 mg) in the morning
Natural Mast Cell Stabilizers: Research and Science
- Lutein helps with “brain fog,” inflammation, and obesity, all of which are important components of neuropsychiatric diseases. (Study – Lutein improves brain “fog,” inflammation, and obesity, three important components of neuropsychiatric diseases.) The same research also found that luteolin prevents mast cells from releasing histamine.
- Palmitoylethanolamide is a fatty acid derived from palmitoyl (works on the endocannabanoid system)
- “PEA’s capacity to regulate MC degranulation via a CB1 CB2 independent mechanism has opened the path for its therapeutic application in both animals and humans. The stabilization of MCs by PEA has been shown to be effective in the treatment of atopic and irritative dermatitis. Finally, we may speculate that cannabinomimetic substances, such as PEA and its congeners, regulate MC activation and degranulation early in the inflammatory response, resulting in a rapid resolution and avoiding the development of chronic inflammatory disease.” (Study)
- (Glia and mast cells as targets for palmitoylethanolamide, an anti-inflammatory and neuroprotective lipid mediator – research) Palmitoylethanolamide is a powerful mast cell stabilizer and pain reliever.
- A powerful neuroinflammation reduction for individuals with various problems, working synergistically inside the endocannabenoid system. Overview/meta analysis, as well as a research of neuroinflammation: N-Palmitoylethanolamine and Neuroinflammation: A Novel Anti-Inflammatory Therapeutic Strategy
- With, luteolin plus palmitoylethanolamide equals even greater stability. PEA and luteolin decrease mast cell-mediated toxicity and elicit neuroprotection in cell-based models of brain ischemia, according to a study. (The Mirica product is seen above.)
- Binders, such as zeolite, are discussed as a way to help mop up histamine here, and there’s a separate article on how zeolite binds histamines here. See also Comparative investigation of histamine-binding capabilities of various natural zeolites.
- Rosae Multiflorae Fructus Hot Water Extract Inhibits a Murine Allergic Asthma Via the Suppression of Th2 Cytokine Production and Histamine Release from Mast Cells – Study – Rosae Multiflorae Fructus Hot Water Extract Inhibits a Murine Allergic Asthma Via the Suppression of Th2 Cytokine Production and Histamine Release from Mast Cells – Study
- Quercetin
- Blocks the release of histamine caused by chemotherapeutic drugs. Quercetin reduces paclitaxel-induced neuropathic pain by stabilizing mast cells and inhibiting PKC-dependent TRPV1 activation, according to a new study.
- Quercetin is also effective for a variety of allergies. The Anti-Allergic Immune Response of Quercetin – a research
- Quercetin works better than sodium cromlyn for stabilizing mast cells in certain conditions. Study: Quercetin Is More Effective than Cromolyn in Blocking Human Mast Cell Cytokine Release and Inhibits Contact Dermatitis and Photosensitivity in Humans.
- The availability of quercetin phytosomes rises, allowing for greater meditator stability and cytokine blocking. “The Quercetin Phytosome formulation showed significant increases in both in vitro solubility and oral absorption (in terms of both exposure and maximum concentration reached) by healthy volunteers in a human clinical trial when compared to unformulated quercetin.”
- Selective Cannabinoid Receptor-1 Agonists Regulate Mast Cell Activation in an Oxazolone-Induced Atopic Dermatitis Model Study – Cannabinoid Receptor-1 Agonists Suppress Mast Cell Histamine Release in an Oxazolone-Induced Atopic Dermatitis Model The research “Cannabinomimetic Control of Mast Cell Mediator Release: A New Perspective in Chronic Inflammation” also found that “cannabinomimetic control of mast cell mediator release: A New Perspective in Chronic Inflammation.”
- Curcumin is also an antihistamine, and when activated, it has been shown to reduce the release of mediators by mast cells:
- Curcumin has an anti-inflammatory impact on mast cells. -mediated allergy reactions in a mouse model of allergic rhinitis produced by ovalbumin (study)
- In mice, lipopolysaccharide (LPS) exposure had a distinct effect on allergic asthma exacerbations and their treatment with intranasal curcumin. (study)
- In a mouse model of food allergy, curcumin inhibits mastocytosis and suppresses intestinal anaphylaxis. (study)
- Curcumin’s inhibitory effects on the passive cutaneous anaphylactoid response and mast cell activation caused by compound 48/80 (study)
- Vitamin C aids in the stabilization of mast cells.
- Alison Vickery’s article on how Vitamin C may help the body produce more DAO, which subsequently eats up histamine.
- Article: Vitamin C, Mast Cells, and Inflammation: “Based on these findings, we may infer that vitamin C alleviates the majority of the symptoms of illnesses involving MC activation, and that further study into the function of vitamin C and MCs is required.”
- “Future research should focus on the use of short-term high-dose intravenous vitamin C as a resuscitation drug in critically ill patients, to intervene as early as possible in the oxidant cascade in order to optimize macrocirculation and microcirculation and limit cellular injury,” according to the article.
- In rats, Nigella sativa (black cumin seed) inhibits mast cell degranulation (Effects of Nigella sativa seeds and specific species of fungus extracts on number and activation of dural mast cells in rats, according to a research.)
- Probiotics that may be beneficial include:
- Lactobacillus G/G: a research project
- This site isn’t excellent, but it lists probiotics that cause histamine release vs those that aren’t: here.
- In certain trials, vitamin E has been shown to reduce mast cell degranulation. (study)
What Cosmetics, Cleaning and Laundry Products, and Toiletries are MCAS-Safe?

Because I’ve lived in both the USA and Canada with this condition, I’m listing out both products from Canada and the United States. This is what I’ve switched to, and this section came about from readers writing in for me to share what’s worked for me.
- For cleaning goods, I use Seventh Generation free and clear all-purpose cleaner.
- In Canada, I use Oneka lavender and angelica shampoo and conditioner (they’re fantastic!). I like lavender, but they also offer unscented alternatives), and in the United States, Andalou Naturals lavender shampoo and conditioner.
- In the United States, I use ECOS lavender washing detergent, while in Canada, I use EcoMax baby laundry detergent.
- In both countries, I use unscented Seventh Generation free and clear laundry drying sheets.
- In Canada, I use Badger Baby SPF 30 Sensitive sunscreen, while in the United States, I use Badger Baby SPF 40 sunscreen.
- For daytime and nighttime moisturizing, I switched to Cliganic Organic Jojoba Oil for the face and eyes, and Jojoba for the face with a few drops of Cliganic Organic Rosehip Oil around my eyes. (These brands are sold in both Canada and the United States.)
- I use REN Clean Skincare Rosa Centifolia Cleansing Gel as a face cleanser (the Amazon review is terrible since someone was upset their face pump didn’t work, but you can check out the REN site for more information). I’ve been using it for years and like it. It does include a little amount of xanthan gum, which may upset some people.
- For makeup, I’ve found Tarte Cosmetics to be the safest for my skin and eyes. I didn’t realize how much my makeup was impacting how I feel until I connected that it was my mascara making my eyes burn and run a lot more than usual. The tinted face cream I used to use also started to give me rashes as I continued on this mast cell journey. I use their Tarte Lights, Camera, Lashes mascara, their Face Tape Foundation, their Amazonian clay blush in Paaarty (I don’t make the names here), and their natural eyeshadow palette. I find their products last a long time, though they are costly. If you wanted to try them out, their website has a lot of mini sizes for you to sample at a lower cost.
- I can’t take Voltaren gel for pain, instead I use Soothamide from Vitalitus, which is made from pharmaceutical-grade palmitoylethanolamide.
- Hello Coconut and Mint toothpaste (the toothpaste does not include any dyes, colors, flavors, SLS/Sulfates, or parabens, but it does contain fluoride). Some mast cell sufferers avoid fluoride since it, too, may raise histamine levels (source), but I use fluoride toothpaste because my teeth have deteriorated owing to MCAS.)
- In Canada, Live Clean Dish Soap is used, while in the United States, ECOS hypoallergenic lavender dish soap is used.
- In Canada, EcoMax hypoallergenic soap is used, while in the United States, ECOS hypoallergenic lavender hand soap is used.
SYNOPSIS OF THIS SECTION ON NATURAL MCAS TREATMENT:
- Natural Mast Cell Stabilizers Research: a) chart (excerpt below) or b) complete research.
PHARMACEUTICAL TREATMENT OF MAST CELLS
In general, an H1/H2 “blockade” is administered every 12 hours. Mast cell stabilizers are also used, as well as pain relievers on occasion.
- H1 blockers (Zyrtec, Xyzal, Claritin, Allegra, hydroxyzine, doxepin, loratadine, fexofenadine) – e.g. Zyrtec, Xyzal, Claritin, Allegra, hydroxyzine, doxepin, loratadine, fexofenadine, hydroxyzine, doxepin, lorat
- H2 obstructors famotidine, Pepcid, Zantac, Tagamet
- Montelukast/Singulair are leukotriene inhibitors.
- Prescription mast cell stabilizers (NOTE: they are not complete mast cell stabilizers since they do not stop cytokine release, but they do have some mast cell stabilizing characteristics and are often prescribed as stabilizers by mast cell physicians.)
- sodium cromolyn
- In the United States, ketotifen is available as an oral, compounded, and prescription drug. In Canada and other countries, Teva produces Zatiden, a ketotifen oral tablet. Many nations, including Mexico, Myanmar, India, and others, sell ketotifen oral pills over the counter. Zatidor eye drops also include ketotifen, but in a fumarate form).
Here’s the link to the research Pharmacological therapy options for mast cell activation disorder, as well as the Hoffman article’s recommendations from the overview part.
The Mastocytosis Society also offers a list of popular pharmacological therapies for mast cell diseases here.
PAIN AND MAST CELLS
In general, pain and mast cell activity are linked (includes tables with treatment options)
(A Practical Guide for Pain Treatment in Patients with Systemic Mast Cell Activation Disease)
Mast cells are the pain gatekeepers throughout the entire pain communication network. Through mediators, mast cells may interact with neurons, glia cells, microglia, and vascular endothelial cells. Through histamine, they have a direct impact on brain processes. As a result, pain alone may cause mast cell degranulation. Through mediators and cytokines, mast cells and the nervous system affect each other’s reactions. Mediators in the periphery may activate receptors, causing discomfort. This promotes mast cell activation, resulting in neurogenic inflammation as a consequence of a feedback loop. Mast cells may attract other immune cells, causing them to produce more mediators and increase inflammation.
Mast cell activation to extremes results in improper mediator release and reactivity, resulting in a wide variety of responses in many tissues and systems. Classical analgesics, most narcotics, and nonsteroidal anti-inflammatory medications (NSAIDS) may all cause MCAD, rendering them useless. (See the “TABLE 4” graphic below.)Study is the source.
Mast cell dysfunction should be addressed by treating the mast cell mediator-related causes of pain perception. However, since pain is one of the most common mast cell triggers, reducing pain levels is critical.
Mast cell stabilizers, avoiding inflammatory foods, and meditation have all helped me and may assist others before turning to harsher medication treatment, particularly because neuropathic pain is so difficult to manage. (Except when I consume/am near anything that irritates mast cells, I went from 24/7 searing agony all over my body to none.)
Mast cells and discomfort are two things that come to mind when thinking about mast cells. EMBRN is the source of this information.
In the event of mast cell activation, neuropathic pain is poorly (if at all) responsive to traditional medication treatment, as indicated in the table below. Furthermore, some of these medications may exacerbate symptoms by boosting mast cell activity even more.
Fibromyalgia Pain and Mast Cells: A 2019 Study
Mast cells are important actors in neuroendocrine and painful diseases, including fibromyalgia, according to a 2019 research, and blocking mast cells may be an effective treatment for fibromyalgia.
The flavonoids luteolin and tetramethoxyluteolin, alone or in conjunction with other drugs chosen to decrease stress, may be used. Palmitoylethanolamide, for example, is a natural chemical that seems to suppress neuroinflammation and relieve pain.” “Mast Cells, Neuroinflammation, and Pain in Fibromyalgia Syndrome,” according to the source.
IBS Pain and Mast Cells (Irritable Bowel Syndrome)
Researchers have discovered the molecular process that they believe may explain why some individuals feel stomach pain when they consume particular foods, according to a paper published in Nature in 2024 titled “Local immune response to food antigens causes meal-induced abdominal discomfort.” The KU Leuven investigations, which were conducted in mice and people, indicate to local mast cell activation. This local immunological response causes pain and discomfort by releasing histamine and other mediators (as detailed on this resource page). The researchers believe these results may open the way for more effective therapies for IBS and other food intolerances, and they are now conducting a bigger clinical study of antihistamine medications.
While severe stomach pain is widespread, the underlying reason is often unknown, according to an open access article that accompanies the research titled “Food for thought regarding the immunological drivers of gut pain.” This new mast cell research suggests that a localized immune response causes usually harmless foods to be misinterpreted as dangerous, resulting in chronic discomfort.
Pain is caused by an immune reaction to an innocuous meal. “A previously undiscovered source of stomach pain,” according to the 2024 research. a, Immune cells in the gut, such as mast cells, which produce histamine molecules, generally don’t attack food or microbes that live there (commensal bacteria). When the gut barrier breaks down (gut cells lose their connection) and food and bacteria leave the gut lumen and enter the body in mice infected with Citrobacter rodentium, immune cells react.
Immune cells release defense chemicals against C. rodentium, as well as antibodies that identify the innocuous food that is there. As a consequence of the infection, pain develops. b, After infection, the intestinal barrier starts to heal. Mast cells become prepared to react by migrating closer to neurons and producing a receptor (derived from the previously created antibody) that detects a food fragment known as an antigen. c,
Mast cells detect the meal after it has been eaten and release histamine via a process known as degranulation. Histamine activates sensory neurons by binding to a receptor on their surface, producing pain.” Nature is the source of this information.
The following is taken from the article:
When compared to healthy people, IBS patients exhibited more mast cells in close proximity to nerve fibers, suggesting a more efficient transmission of information between mast cells and sensory neuron nerve ends.
And recommends that, as a consequence of the findings of this research, future therapies for IBS may include:
- reducing gut permeability to decrease gut access to the intestinal immune system (this is what ‘leaky gut’ healing is all about);
- IgE antibodies specific to the dietary item of interest are targeted;
- decreasing mast-cell degranulation (this page’s focus! );
- targeting mast cell-released particular chemicals; and
- colonic sensory nerves that convey information and produce pain are blocked.
INFLAMMATION IS INCREASED BY MAST CELLS IN WHAT WAY?
Low inflammatory and low histamine diets may be beneficial, as explained in this section.
- Dr. Theoharides thinks that CRH causes mast cells in the hypothalamus (and elsewhere) to generate a substance called vascular endothelial growth factor (VEGF), which enhances blood-brain barrier permeability (BBB). More immune cells (e.g. mast cells) and perhaps pathogens infiltrate the brain as a result of the leaky BBB, and inflammation ensues. Could Mast Cells in the Brain Be Causing Chronic Fatigue Syndrome (ME/CFS)?
- Mast cells function as both sensors and effectors, allowing the neurological, vascular, and immune systems to communicate. They reside on the “brain side” of the blood-brain barrier in the brain, where their mediators and molecules interact with astrocytes, microglia, and blood vessels. They are the body’s initial responders, accelerating reactions, enhancing responses, and, once engaged, attracting other immune responses. This contributes to neuroinflammation when it is dysregulated. See also the following research.“Mast cells contribute to normal behavioral functioning, especially cognition and emotion, while also promoting negative consequences in brain function. Mast cells may play a significant role in the treatment of systemic inflammation or the blocking of peripheral-to-brain communication pathways.” Mast Cells and Neuroinflammation“, Mast Cells and Neuroinflammation, Mast Cells and Neuroinflammation, Mas
- Brain traumas, neuropsychiatric diseases, stress, neuroinflammation, and neurodegeneration have all been linked to mast cells. Mast Cell Activation in the Pathogenesis of Alzheimer’s Disease and Brain Injury, Stress, and Post-traumatic Stress Disorder
- Neurogenic inflammation may be caused by increased contact between mast cells and nerves. Mast cell numbers have risen significantly in inflammatory models, resulting in enhanced release of inflammatory mediators upon degranulation.“Through the activation of receptors on nerve terminals, inflammatory mast cell mediators may regulate sensory neurons. […] As a consequence, mast cell activation may enhance sensory neuron excitability as well as neuropeptide synthesis and secretion.” Source: “The Importance of Mast Cell-Nerve Communication”
- Mast cells are important in peripheral inflammation as well as neuroinflammation caused by brain injury, stress, depression, and post-traumatic stress disorder (PTSD). As a result, mast cell activation in the context of brain damage, stress, and PTSD may hasten the onset of neuroinflammatory and neurodegenerative illnesses such as Alzheimer’s disease. Mast cells in brain traumas, stress, and PTSD may have a role in Alzheimer’s disease pathogenesis. “We believe that inhibiting mast cell activation and brain cell-associated inflammatory pathways in brain traumas, stress, and PTSD may be investigated as a novel therapeutic target to delay or prevent Alzheimer’s disease etiology and severity.” Mast Cell Activation in the Pathogenesis of Alzheimer’s Disease and Brain Injury, Stress, and Post-traumatic Stress Disorder
- Mast cell disorders: From childhood through adulthood: “Mast cells are also taking on a novel role in severe asthma and blood vessel remodeling in cancer and atherosclerotic vascular disease. Furthermore, new data indicates that mast cells detect changes in oxygen tension, especially in newborns, and that subsequent degranulation may contribute to prevalent preterm lung, eye, and brain disorders traditionally linked to hypoxic insults.” Mast cell diseases and chronic inflammatory illnesses involving mast cell dysfunction are discussed in this article.
CELIAC DISEASE AND MAST CELLS
- [Study] Mast cells are linked to the development of celiac disease. “We describe the phases of Celiac Disease as they develop, with mast cells as the hallmark of the inflammatory process. As a result, the current understanding of Celiac Disease must be updated, and the role of mast cells in the development and progression of Celiac Disease must be addressed when creating novel treatment approaches.”
- [Study] Intestinal mast cell involvement in celiac disease.
- A review of research looking at the function of mast cells in the pathogenesis of celiac disease, revealing that these cells grow in number as the illness progresses and help to establish a pro-inflammatory milieu. [study] “To summarize, mast cells are thought to be one of the major actors in intestine damage during the development of Celiac Disease. As a result, the etiology of Celiac Disease should be reconsidered, and the role of mast cells in the disease’s development and progression should be addressed when developing novel treatment approaches.”
- Mast cells are also implicated in dermatitis herpetiformis, which is a persistent, itchy, blistering skin disorder caused by celiac disease. Although dermatitis herpetiformis does not cause the same gastrointestinal symptoms as celiac disease, it is nonetheless related. Mast cells that have gone wild will cause tissue damage by generating excessive inflammation. This pattern has been linked to diseases such as dermatitis herpetiformis in studies.
EHLERS DANLOS SYNDROME AND MAST CELLS (EDS)
The astonishing frequency of mast cell problems among leakers was one of the factors that prompted me to create this article. People with connective tissue dysfunction or some other genetic and/or pathogenetic cause for the body’s inability to seal and repair the dura robustly, even with assistance, make up the majority of that group.
Continuous mast cell degranulation, it turns out, may harm connective tissue, which is a double whammy for individuals with connective tissue diseases. When a mast cell degranulates, it releases not just histamine but also proteases, which are enzymes that break proteins down into smaller polypeptides or single amino acids. Mast cells may damage tissue integrity over time since they reside in tissues all throughout the body.
EDS is a hereditary connective tissue disease caused by mutations in collagen or other extracellular matrix proteins (ECM). The ECM is a network that keeps tissues together, so when mast cells degranulate and disrupt that network, it may cause permeability in the gut lining, as well as increased tissue laxity and/or hypermobility symptoms, according to research.
As a result, mast cell illness may have impacts on the whole body’s connective tissue, particularly if you have a pre-existing hereditary condition.
- – this research investigates if the fact that mast cells reside in connective tissue, coupled with the “wonky” connective tissue of EDSers, implies that mast cell activation is more frequent due of the alterations in connective tissue structure in mainly hEDS patients. Doctor Maitland and Doctor Afrin’s whole study is available online.
- Mast cells undergo greater modification when they are affected by surrounding cells after being recruited to connective tissues. And our connective tissues are home to a large number of mast cells. This research investigates how mast cell dysregulation arises in connective tissue diseases.
MAST CELLS AND DIFFERENT TYPES OF SCLEROSIS (MS)
- The author of a review article titled Curbing Inflammation in Multiple Sclerosis and Endometriosis: Should Mast Cells Be Targeted? discusses how many inflammatory diseases are fueled by both internal and external stimuli, begin as inflammation, and then progress to a disease state after tissue damage and other factors. Depending on the illness, many different cell types are involved, but mast cells are typically one of them (in both the acute inflammation and in the disease state). “Recent investigations in pig and rabbit models have supported the notion of a pivotal function for mast cells in a “nerve-mast cell-myofibroblast axis,” according to the paper, with mast cells playing a key part in the disease-causing inflammatory process.
Elevated levels of mast cell products have been detected in fluids from MS patients. These include mast cell tryptase in CSF from MS patients and histamine levels in CSF from MS patients. In spite of such evidence, the role of mast cells in MS is still somewhat controversial.
Targeting mast cells in both MS and endometriosis, the study adds, “may be a productive route to manage the recurrent inflammatory exacerbations of the conditions.”
- Neuroinflammation is now well-established as a primary pathological component of diseases such as multiple sclerosis, and is gaining acceptance as an underlying component of most, if not all, neurodegenerative diseases, according to a study published in April 2019 called Mast Cells in Neurodegenerative Disease. Mast cells influence both their microenvironment and neighboring cells such as T cells, astrocytes, microglia, and neurons. Previously, studies concentrated on glial cells of the central nervous system, but now researchers are looking at mast cells as well. They may also disrupt and modify the blood-brain barrier’s permeability, which “has the potential to significantly alter the neuroinflammatory state,” according to the research.
- The 2017 paper Role of Mast Cells in the Pathogenesis of Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis examines how mast cells may promote demyelination in the early stages of ME or EAE. According to the findings, mast cell depletion or limitation may be a new potential treatment target for MS and EAE.
- In another research from 2024, the connection between mast cells and angiogenesis in multiple sclerosis is discussed.
- A research titled “The Importance of Mast Cells in Multiple Sclerosis” was published in 2016. Autoimmunity is a condition in which the body’s immune system attacks its own tissues. Multiple sclerosis (MS) is an autoimmune disease that causes progressive and long-term neurological symptoms. MS is linked to an aberrant B-cell response as well as an increase in T-cell reactivity to a variety of antigens. Mast cells are the first line of defense in the innate immune system, secreting chemical mediators and cytokines after degranulating. Since the turn of the century, their impact on the central nervous system has been identified. They play a key role in autoimmune diseases like MS, mediating inflammation and demyelinization by presenting myelin antigens to T cells or breaking the blood-brain barrier, allowing inflammatory cells and cytokines to enter. Mast cell involvement in MS is shown by chemical mediator and inflammatory cytokine gene overexpression. Mast cells and multiple sclerosis are discussed here in terms of their connection and participation.
COVID-19, LONG COVID, AND MAST CELLS
This section is included since we’ve seen a number of articles on long-COVID / PAS-C and its effects on the body. Some mast cell specialists think that malfunctioning mast cells are to blame for a portion of long-term COVID symptoms. The result of a September 2024 research by physicians Afrin, Weinstock, and Molderings reads:
Within the Covid-19-infected population, the incidence of MCAS is comparable to that of severe cases. Much of Covid-19’s hyperinflammation is similar to the types of inflammatory that may be induced by MC activation. Preliminary evidence suggests that drugs that target MCs or their mediators may be beneficial to Covid-19 patients. None of the authors’ MCAS patients who were treated with Covid-19 developed serious infection, much alone died.
The FDA has approved an IL-6 inhibitor for patients with severe COVID-19. https://t.co/qycJmkixXN After SARS-CoV2 infection, where does the Il-6 come from? #Mastcells are an immunological cell that is often overlooked.
June 26, 2024 — Anne Maitland, MD (@asktheallergist)
Please also have a look at:
Mast Cells and COVID-19: a Case Report suggesting a function of mast cell activation in the prevention and treatment of Covid-19 also follows a patient.
She had a lengthy history of symptoms that were concerning for a mast cell activation syndrome (MCAS), but she had never received test proof of this non-clonal mast cell activation disease until she acquired COVID-19. This example highlights the need of determining the rate of mast cell activation in SARS-CoV-2 infection, not only to improve anti-SARS-CoV-2 treatment, such as vaccine development, but also to reduce the risk of SARS-CoV-2-induced hyperinflammatory syndrome.
As new information becomes available, I will update this area.
STUDIES HAVE LINKED OTHER CONDITIONS TO MAST CELL DYSFUNCTION.
Mast cells have been linked to IBS, fibromyalgia pain, and a few other diseases, according to research. Mast cells have also been linked to a number of different health problems. This isn’t to say that having those circumstances implies you have a mast cell problem; rather, inhibiting mast cells may successfully relieve some of the disease’s symptoms. For some of those diseases, I’ve included links to papers or review articles below.
When you consider that mast cells may be located all throughout the body and in the brain, it’s easy to see how they might play a role in a number of diseases involving the neurological system, immune system, or tissues. Among them are the following:
- Vulvodynia (also known as interstitial cystitis) may be found here and here.
- See here and here for more information about interstitial cystitis.
- See here for more information about Postural Orthostatic Tachycardia Syndrome.
- See this page for more information about osteoarthritis.
- See this page for information on chronic hives and itching.
- See this page for more information about Restless Leg Syndrome.
- See here and here for more information about peripheral neuropathy. (I often get severe tingling and burning in my hands and feet during bad flares.)
- See here for information on allergic illnesses such as asthma and atopic dermatitis (among others).
- Endometriosis – check the MS section for further information, as well as here.
- Arthritis may be found here.
- Migraines may be found here, along with a complete research.
- See this page for more information about trigeminal neuralgia.
- See this page for more information about asthma.
Patients with interstitial cystitis and/or vulvodynia may benefit from a low-oxalate diet, according to the pelvic pain and vulvodynia foundations. (See this page for further information.) The diet is outlined in the section above under “naturally treating mast cells.”
SLEEP, MAST CELLS, AND JET LAG

Does this page sound very familar to you, and you also have a terrible time with sleep? You’re not alone. Mast cell research has shown that the cells are controlled by their own “internal clock”, regulated by clock genes just like other organs in the body. This circadian clock regulates many things in the body, and since mast cells themselves have a circadian expression, it’s important to look at them when it comes to sleep as well.
Mast cells are influenced by their clock genes, as well as the other variables discussed in this article, such as food, triggers, and hormones. In addition, histamine is involved in the sleep-wake cycle control. Mast cells have an important role in both sleep and wakefulness.
Until I had my mast cells under control, I had horrible sleep for the most of my life. Before going to bed, my mind would race, keeping me up all night. Attempts to go asleep were fruitless until 4-5 a.m. since my mast cell problems worsened with the beginning of the CSF leak. I used to be fully awake or, if I began to doze off, I would gasp awake, literally pulling my body away from sleep. Of course, this was not done on purpose, and I mistook it for worry.
But it turns out that I didn’t have the anxiousness I thought I had. It was a huge physiological shift. I was able to sleep again after using the above-mentioned procedure. I was no longer experiencing myoclonic twitches before falling asleep. Before going to bed, I didn’t have to cope with racing thoughts. If I did manage to fall asleep, I was no longer waking up at 4 a.m.
It turned out that the problem had all along been mast cell problems. This makes logical since histamine impacts both sleep and waking cycles, peaking about 3 a.m. It also promotes alertness, so if it’s abnormally high in someone with a mast cell disease, where it’s not produced properly or in excess, sleeplessness (along with a racing heart, changes in temperature, blood pressure, and flushing) is likely.
For additional information, read my in-depth essay on jet lag, mast cells, and immune cells, which includes a detailed jet lag regimen for minimizing circadian rhythm disturbance in daily life as well as while flying.
Chronotherapy with COVID-19

Scientists are increasingly turning to the body’s circadian cycle to assist manage current illnesses and therapies in the future.
“We wanted to completely understand why this medication was helpful to some individuals but had bad effects on others when we observed the debate around the usage of ibuprofen,” said Harry Karmouty-Quintana of University of Texas Health. Harry’s team suggests giving anti-inflammatory medicine at specific times of the day in a report published in the British Journal of Pharmacology called The case for chronotherapy in Covid19-induced acute respiratory distress syndrome, which would affect the body’s response to the medication without interfering with its fight against COVID-19.
The research adds, “We believe that the intrinsic circadian clock of the lung and immune system may control separate components of CRS, and therefore, chronotherapy may be utilized to successfully treat ARDS in COVID19 patients,” which ties in well with the mast cell sections below. Mast cells have their own circadian cycle, and as they degranulate, they produce cytokines (release inflammatory substances into the blood). According to Harry’s team, giving medicine depending on the timing of the inflammatory surge may help the body recover faster.
As stated in the conclusion:
“This means that the best time to take a medication is in the afternoon, and that taking it at night should be avoided. This is especially essential when delivering immune modulators, which are typically given in a single dosage. Furthermore, the aim of COVID19 chronotherapy is to prevent attaining steady-state medication levels, which, like antiinflammatory therapy, would suppress the virus-directed inflammatory response.”
Based on what doctors know about the circadian clock of immune cells, they think that time timing of anti-inflammatory agents are important. This is because the immune cells release cell signals associated with negative effects to the body during the mid-to-late afternoon, but release antiviral molecules during the night and into the early morning. A “therapeutic window” for medication would give the medication an opportunity tamp down on inflammation that harms, while also allowing immune cells to produce the inflammatory molecules needed to fight the virus at night.
CALMING MAST CELLS WITH NON-CONVENTIONAL TREATMENTS
- Breathing techniques: pranayama breathing (PDF) or Butyeko breathing (introduction here):
- Carbon dioxide treatment of mast cells inhibits degranulation via a new mechanism involving suppression of elevated intracellular calcium levels. [Study breathing raises CO2 levels]
- Insights into Hypercapnic Yoga Breathing Exercises: Evidence-Based Role of Hypercapnia and Exhalation Phase in Vagus Nerve Stimulation [Study article – “Research has revealed that vagal stimulation not only helps you regulate the health of your organs and tissues, but it also controls the development of your stem cells, which, in turn, helps your body repair and replace damaged cells”]
- If you’re new to meditation, check out my 10-week free course with guided tracks for beginners.
- In the regulation of neurogenic inflammation, a comparison of mindfulness-based stress reduction and active control [research]
- The benefits of meditation and vacation on disease-related molecular phenotypes [research]
- Dynamic Neural Retraining System is a system that allows you to retrain your brain in a Some mast cell specialists suggest DNRS as a way to reduce overall stress and sensitivity to stimuli, not to ‘treat’ MCAS (which has no cure), but to assist reduce the body’s overall load. This is a neuroplasticity-related technique that is not without dispute.
- Somatic experience therapy (SET) or EMDR (Eye Movement Desensitization and Reprocessing)
- Intermittent fasting is a kind of fasting that occurs on a regular basis Multi-day water fasts are not advised since histamine levels begin to rise again after too much fasting. Restriction of meals to an 8-hour or 6-hour window, on the other hand, seems to be beneficial.
ADDITIONAL READING
The two most useful mast cell books I’ve read are:
DISCLAIMER: The content on this website is designed to offer general health information only and is not intended to replace professional medical advice or treatment from a personal health practitioner. Legal Nomads maintains this website as a personal site and makes no explicit or implied warranties or claims as to the truth or completeness of any views, advice, services, or other material included or references given. Although the site is updated on a regular basis, it may not always represent the most up-to-date information. Because this is not a medical site and is only provided for information based on personal use of the studies and goods described below, any email contact or use of the material on this website does not establish an advisor-patient relationship.
Mast Cell Activation Syndrome (MCAS) is a complex condition causing inflammation of the skin, eyes and breathing passages. Symptoms of MCAS are similar to hay fever, asthma, allergies and even asthma. The main key feature of MCAS is the inflammation of the skin, eyes and breathing passages. In the past, mast cells were believed to be only found in the immune system and were thought to be involved with allergies. However, recent studies show that these cells are present in many parts of the body and are important in protecting against infections.. Read more about can mast cell activation syndrome go away and let us know what you think.




